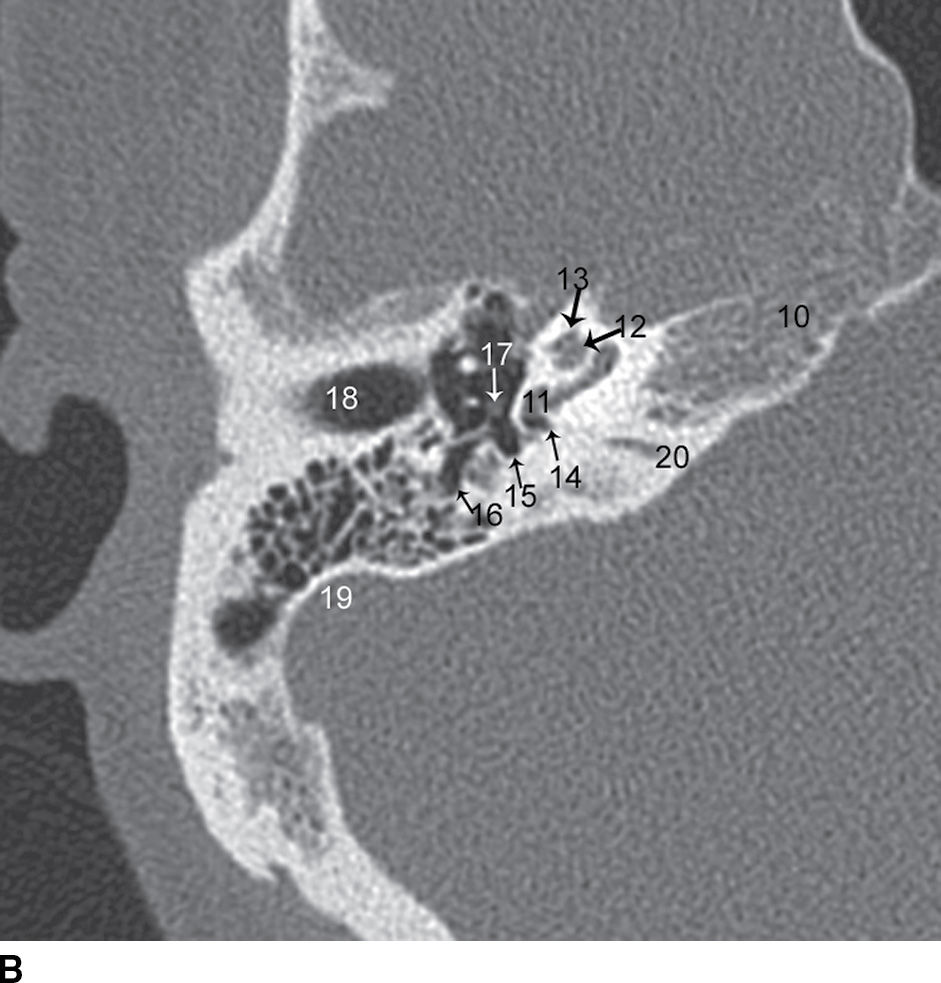
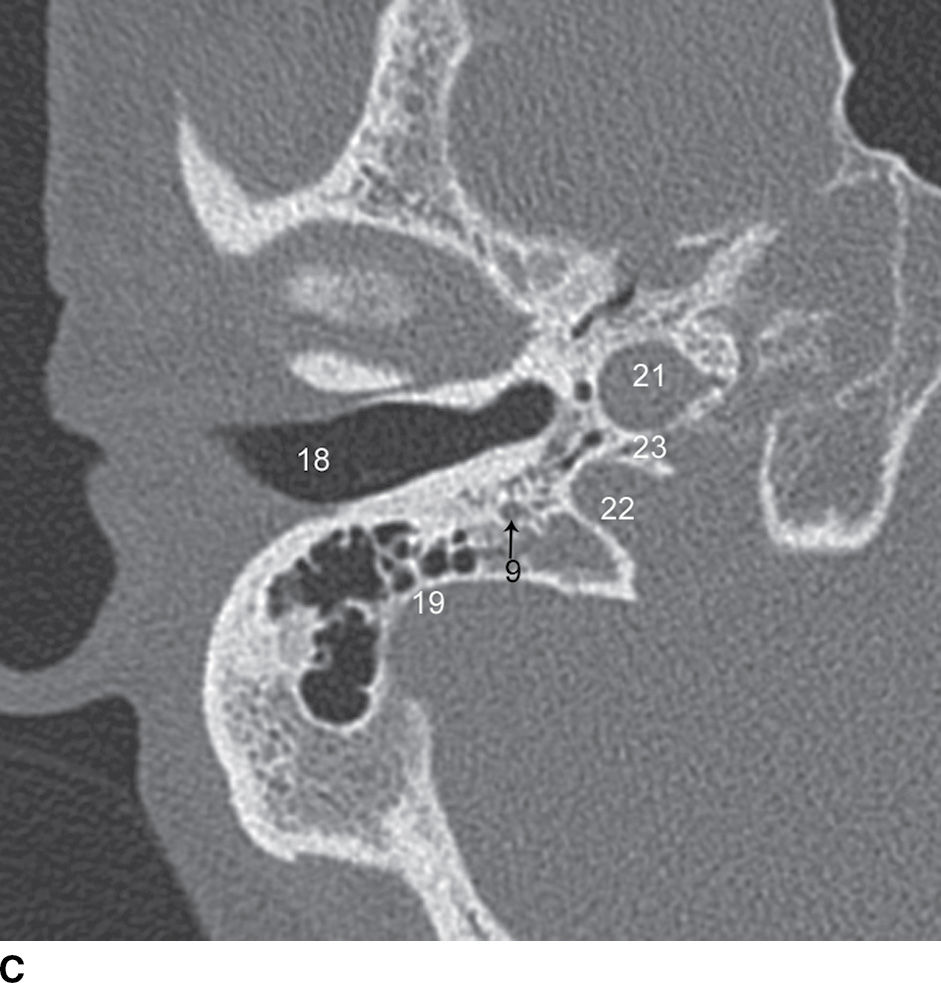

FIG. 20.1 Normal axial CT anatomy. A: Axial image through the mesotympanum shows the following: 1, internal auditory canal; 2, cochlear aperture; 3, vestibule; 4, vestibular aqueduct; 5, posterior semicircular canal; 6, malleus head; 7, incus body; 8, anterior epitympanic recess; 9, facial nerve canal tympanic segment; 10, petrous apex. B: Axial image slightly lower shows the following: 10, petrous apex; 11, basal turn of the cochlea (image label near the cochlear promontory); 12, middle turn of the cochlea; 13, apical turn of the cochlea; 14, round window niche; 15, sinus tympany; 16, facial recess; 17, stapes crura (the incus long process and malleus handle are also visible on this cut); 18, external auditory canal; 19, sigmoid sinus plate; 20, cochlear aqueduct. C: Axial image through the skull base shows the following: 9, facial nerve canal mastoid segment; 18, external auditory canal; 19, sigmoid sinus plate; 21, carotid canal; 22, jugular fossa; 23, caroticojugular spine. D: Coronal image through the middle ear shows the following: 1, internal auditory canal; 3, vestibule; 7, incus long process and lenticular process; 9, facial nerve canal tympanic segment; 18, external auditory canal; 24, lateral semicircular canal; 25, superior semicircular canal; 26, oval window; 27, scutum; 28, Prussak space; 29, tegmen tympani.
MR anatomy
MRI anatomy of the temporal bone/IAC is generally more straightforward than is CT anatomy. The middle ear structures are generally of less importance, as they are better evaluated by CT. The key structures to identify on MRI are facial nerve (cisternal and IAC segments); vestibulocochlear nerve; labyrinthine structures (cochlea, vestibule, semicircular canals); sigmoid sinus; jugular bulb; and internal carotid artery (Fig. 20.2).
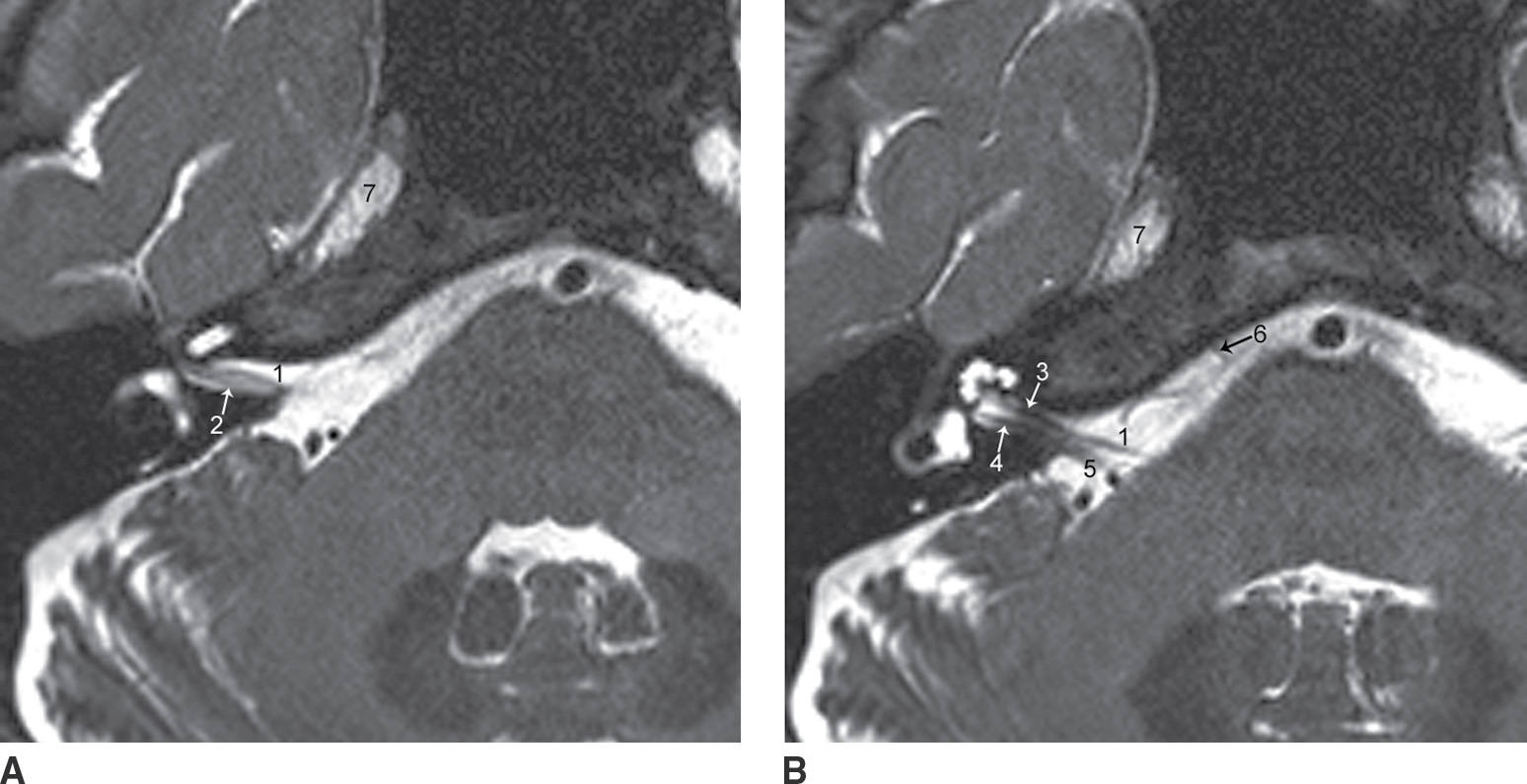
FIG. 20.2 A,B: Normal MR anatomy. Adjacent axial images from a cisternographic T2-weighted sequence show normal appearance of the following: 1, facial nerve; 2, superior vestibular nerve; 3, cochlear nerve; 4, inferior vestibular nerve; 5, vestibulocochlear nerve main trunk; 6, abducens nerve; 7, Meckel cave.
Temporal Bone Emergencies
Trauma and infection are two common indications for temporal bone CT in the emergency setting. The decisions to admit or discharge, to obtain further imaging, or to do surgery often depend on the interpretation of these imaging studies. It is therefore important to be able to recognize and accurately describe a few key processes and to earn the trust of the referring physician through a concise description of the pertinent positive and negative findings.
Trauma
Temporal bone injury may result from blunt trauma to the head. The key findings to look for are fracture and ossicular chain dislocation. If a fracture is present, it is important to carefully assess which structures are involved. Temporal bone fractures are classically divided into longitudinal (parallel to the long axis of the temporal bone) or transverse (perpendicular to the long axis), though most have components of both and are properly described as mixed fractures. More importantly, the ordering physician wants to know whether the fracture traverses the otic capsule, involving the labyrinth or facial nerve canal (Fig. 20.3), and whether the fracture traverses major vascular channels: the carotid canal, sigmoid sinus plate, and jugular fossa (2). If the fracture does traverse major vascular channels, then CTA is typically warranted. Ossicular chain dislocation most commonly involves the malleoincudal joint or the incudostapedial joint (Fig. 20.4). When malleoincudal dislocation is present, the usual “ice cream cone” appearance will be lost. Incudostapedial dislocations can be difficult to detect, but are best seen by looking for an abnormal orientation of the long process of the incus.

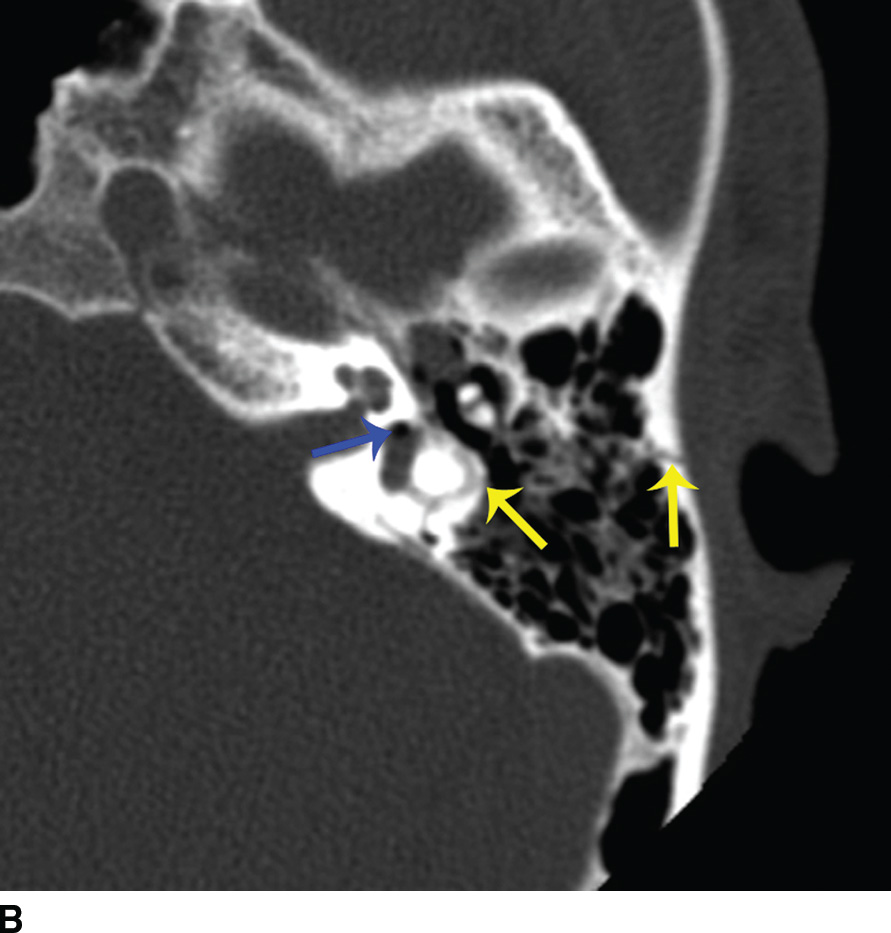
FIG. 20.3 Temporal bone fractures. A: Axial CT image shows a fracture line oriented along the long axis of the temporal bone (arrows), that is, a longitudinal fracture. These fractures typically do not traverse the otic capsule, but do sometimes traverse the carotid canal or jugular fossa, and are also frequently associated with ossicular dislocation. B: Axial CT in a different patient shows a transverse fracture (yellow arrows), traversing the labyrinth, with associated intralabyrinthine air (blue arrow). There is also a subtle ossicular dislocation, with widening of the malleoincudal joint.

FIG. 20.4 Malleoincudal dislocation. Axial CT shows gross disruption of the malleoincudal joint (arrow), with loss of the normal “ice cream cone” relationship of the malleus head (ice cream) and incus body (cone).
Infection
Otitis externa and acute otitis media (AOM)/mastoiditis are two entities that are imaged with temporal bone CT in the emergency setting. When evaluating otitis externa, the ordering physician is looking for signs of malignant otitis externa (MOE). Erosion of adjacent bone, or infiltration of the fat in the infratemporal fossa, is a sign of MOE (Fig. 20.5) (3). In the setting of AOM or mastoiditis, the ordering physician is looking for signs of coalescent otomastoiditis and its associated complications, which include subperiosteal abscess, epidural abscess, and sigmoid sinus thrombosis (Fig. 20.6) (4). Destruction of mastoid trabeculae and erosion of the sigmoid sinus plate are the key findings of coalescent mastoiditis. When these findings are present, contrast-enhanced imaging (either CT or MR) should be recommended to assess for abscess or venous thrombosis.

FIG. 20.5 Malignant otitis externa. Axial CT shows opacification of the right mastoid air cells and infiltration of the fat in the infratemporal fossa (black arrow). Compare to the normal fat in the left infratemporal fossa (white arrow).
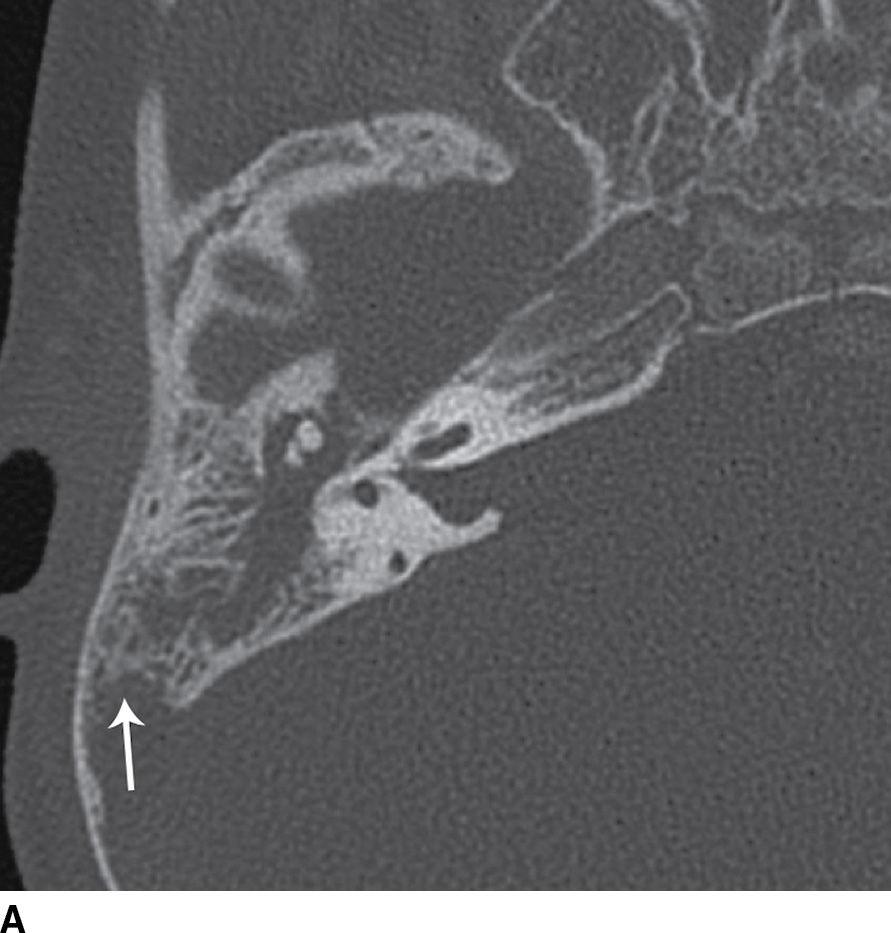
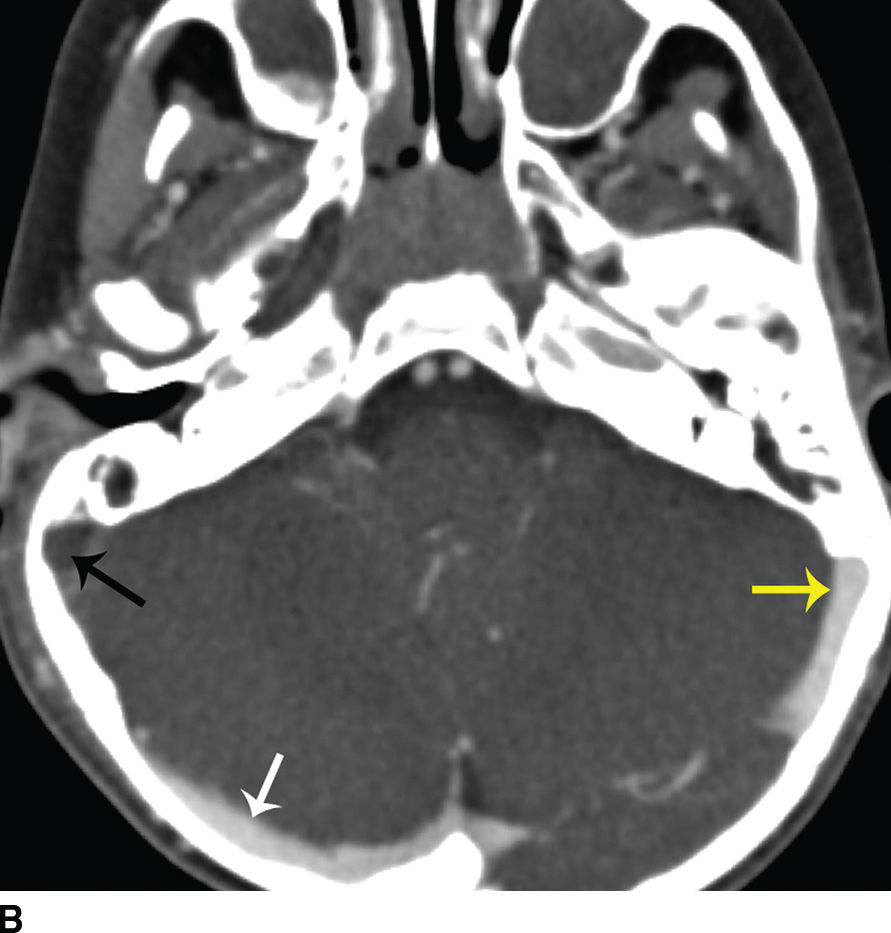
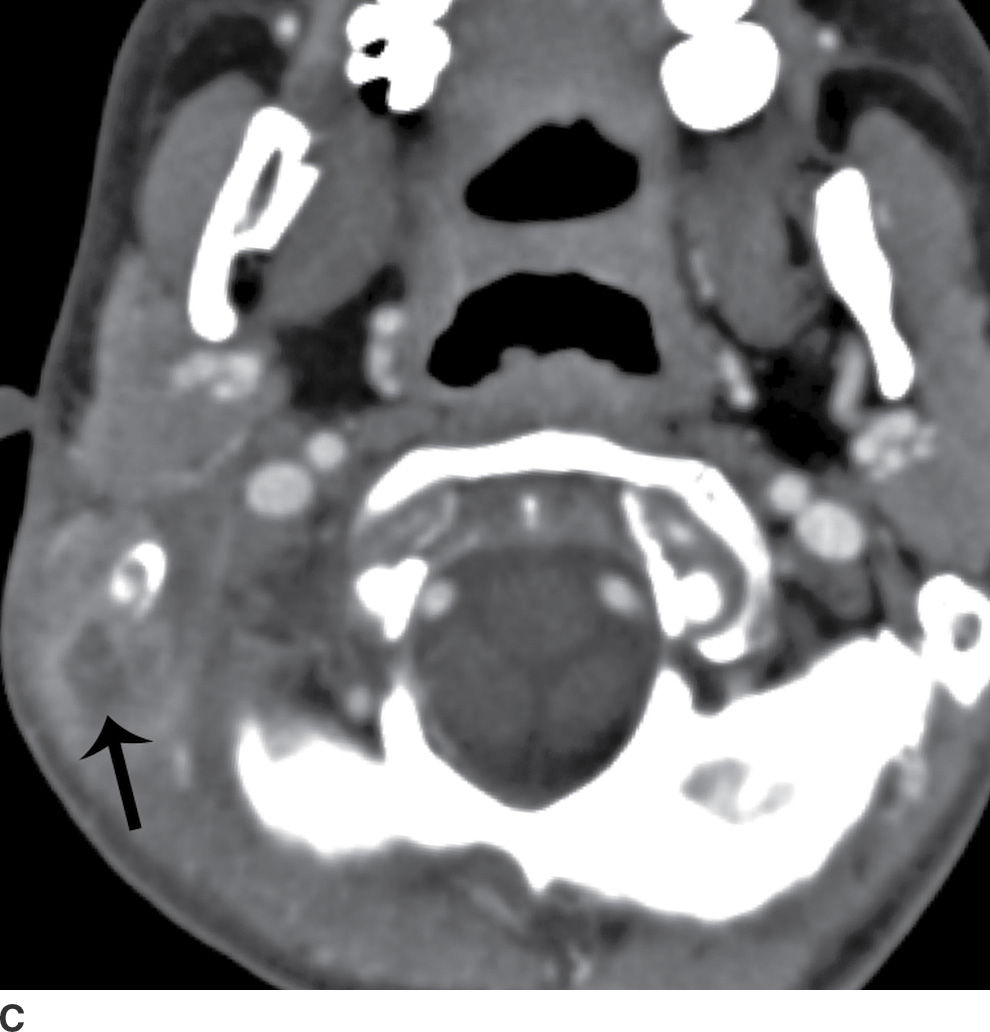
FIG. 20.6 Coalescent otomastoiditis. A: Axial CT in bone windows shows opacification of the mastoid and middle ear. Erosion of the sigmoid sinus plate (arrow) is indicative of coalescence. B: Axial contrast-enhanced CT at the same level as (A) shows a filling defect at the junction of the right transverse and sigmoid sinus (black arrow), indicative of venous sinus thrombosis. Compare to the patent proximal right transverse sinus (white arrow) and contralateral transverse sinus (yellow arrow). C: Axial contrast-enhanced CT at the level of the mastoid tip shows a peripherally enhancing subperiosteal abscess (arrow). Because this abscess is deep to the sternocleidomastoid muscle, it is at higher risk of rupture into the paravertebral space. An abscess in this location is termed “Bezold abscess.”
Outer Ear Disease
Cerumen buildup in the EAC is the most common abnormality of the external ear and is readily detected by the otolaryngologist. When imaging is requested, it is typically to assess other lesions. Malignancy, typically squamous cell carcinoma, may involve the EAC, presenting as a nonspecific contrast-enhancing soft tissue mass. In these cases, imaging is used to assess the extent of disease and for bone erosion. Bony overgrowths, called exostoses (Fig. 20.7), may involve the bony EAC, typically in response to chronic cold water exposure (“surfer’s ear” or “swimmer’s ear”). Rarely, trapped inclusions of squamous epithelium may produce an expansile, destructive mass in the outer ear, which is called cholesteatoma. These lesions are discussed further below. An inflammatory soft tissue mass without bone erosion, called keratosis obturans, may also obstruct the EAC (5).
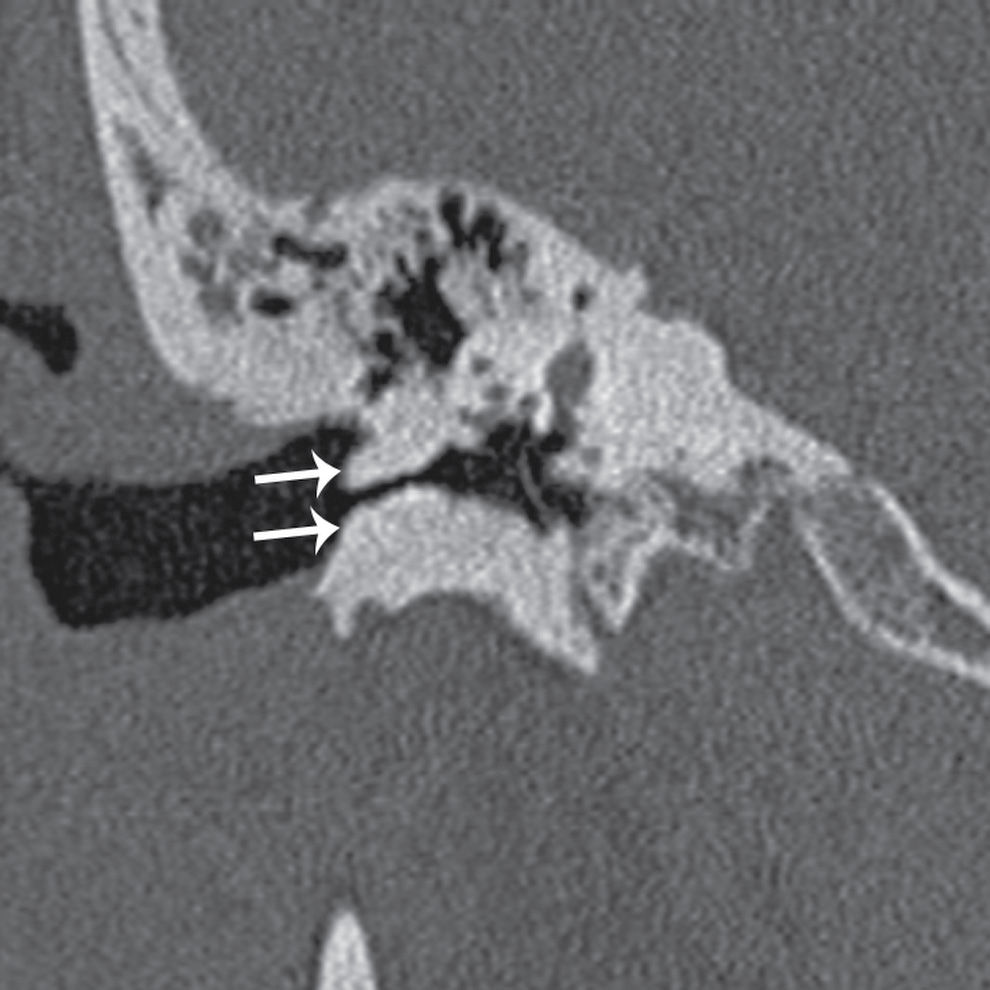
FIG. 20.7 Exostoses. Coronal CT shows prominent bony excrescences from the bony external auditory canal (arrows) that narrow it.
Middle Ear Disease
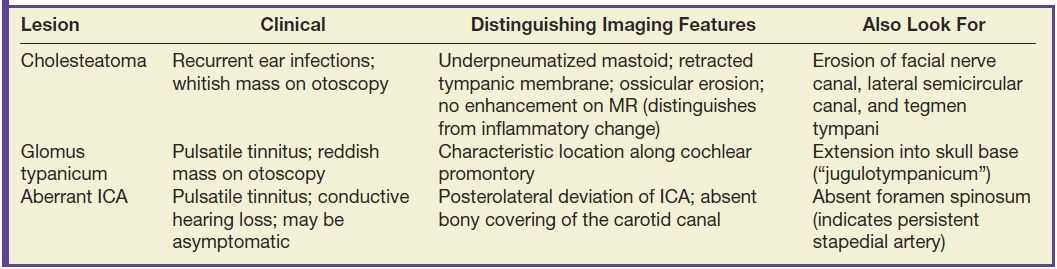
Infection, inflammatory disease, and tumors of the middle ear are commonly evaluated with imaging. Imaging may be performed to work up symptoms such as CHL, pulsatile tinnitus, or otorrhea and to better evaluate a retrotympanic mass detected by otoscopy. The common middle ear mass lesions are discussed here and summarized in Table 20.1.
Table 20.1 Middle Ear Masses
Conductive hearing loss
Otitis media
Otitis media (OM) is a blanket term that describes any inflammation of the middle ear, regardless of etiology, pathogenesis, or disease course. AOM, more common in children than adults due to the more horizontal course of the eustachian tube, typically occurs in a well-pneumatized mastoid. The infectious complications described above are complications of AOM. Chronic OM typically occurs in a mastoid that is underpneumatized due to chronic eustachian tube dysfunction. Cholesteatoma is a more common complication of chronic OM (6). Tympanic membrane thickening may be present, with or without superimposed perforation.
Tympanosclerosis
Calcification of the tympanic membrane may occur as a result of chronic inflammatory disease (Fig. 20.8). The normal tympanic membrane is barely perceptible, whereas a calcified tympanic membrane will be quite prominent despite only minimal thickening (6).

FIG. 20.8 Tympanosclerosis and labyrinthitis ossificans. Axial CT shows evidence of a prior canal wall up mastoidectomy. The tympanic membrane is calcified (white arrow), and there is also hazy density in the basal turn of the cochlea reflective of labyrinthitis ossificans (black arrow).
Otosclerosis
Otosclerosis is a metabolic condition of unknown etiology that produces abnormal resorption of bone. The normally dense bone becomes spongiotic; hence the preference for the term “otospongiosis” by many radiologists. The bony protuberance just anterior the oval window, the fissula ante fenestram, is characteristically the first site of involvement (Fig. 20.9). Rarefaction of the spongiotic bone in this region inhibits motion of the stapes footplate, leading to CHL, which is treated with stapedotomy or stapedectomy. Tinnitus is also common early in the disease course. Otosclerosis is bilateral in 85% of cases. Spongiotic change may also involve the otic capsule in approximately 15% of cases, characteristically starting just posteromedial to the basal turn, termed retrofenestral or cochlear otosclerosis. This is associated with SNHL and generally only occurs in patients who already have fenestral otosclerosis (7).
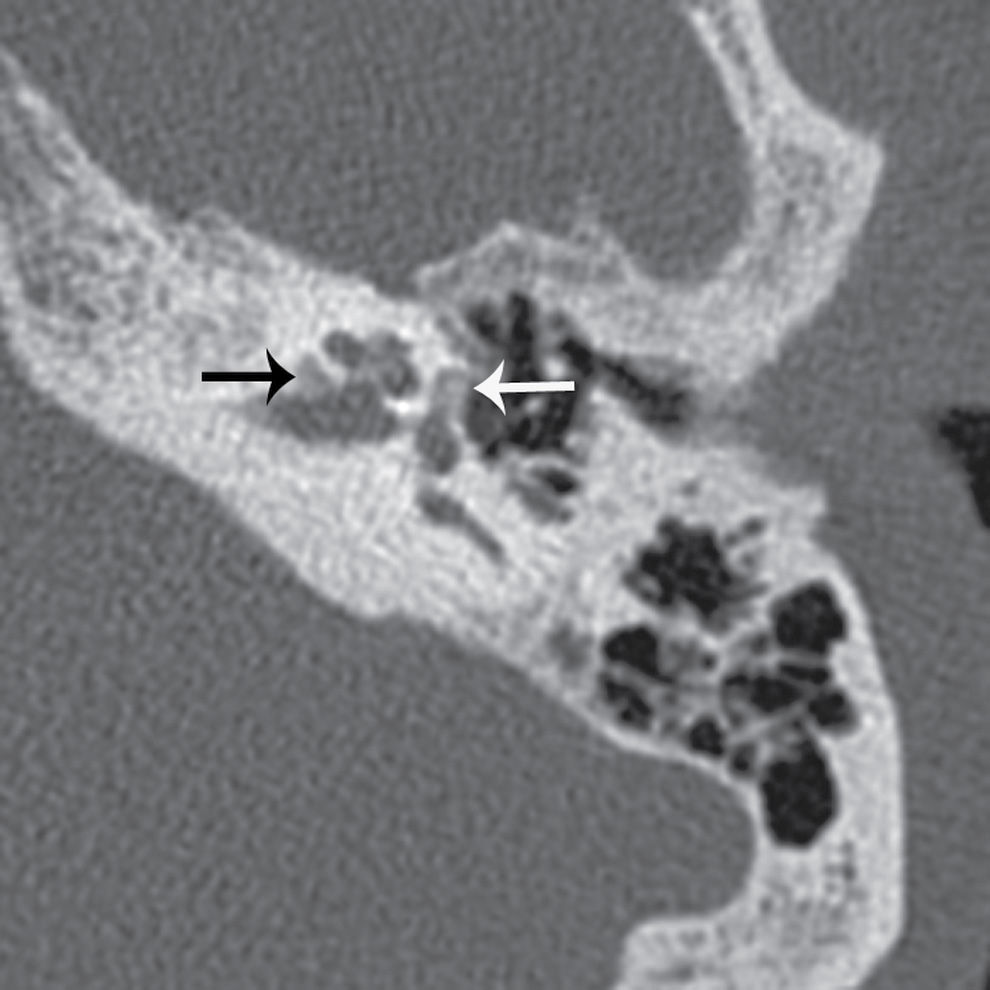
FIG. 20.9 Otosclerosis, fenestral and retrofenestral. Axial CT through the level of the vestibule shows abnormal lucency anterior to the oval window (white arrow), involving the fissula ante fenestram. This is termed “fenestral otosclerosis” and typically produces conductive hearing loss through inhibition of stapes motion. There is also abnormal lucency posteromedial to the basal turn of the cochlea (black arrow), termed “retrofenestral otosclerosis,” which is sometimes associated with sensorineural hearing loss.
Semicircular canal dehiscence
The normal sound-induced pressure wave is conducted from the tympanic membrane, through the ossicles to the oval window, and is decompressed through the round window. When the bony covering of one of the semicircular canals, usually the superior canal, is deficient (Fig. 20.10), the sound-induced pressure wave may be partially decompressed through the vestibular system, leading to CHL and symptoms such as autophony, vertigo, and nystagmus. Tullio phenomenon is the name given to vestibular symptoms provoked by loud sounds. The primary clinical differential for semicircular canal dehiscence is otosclerosis (8).
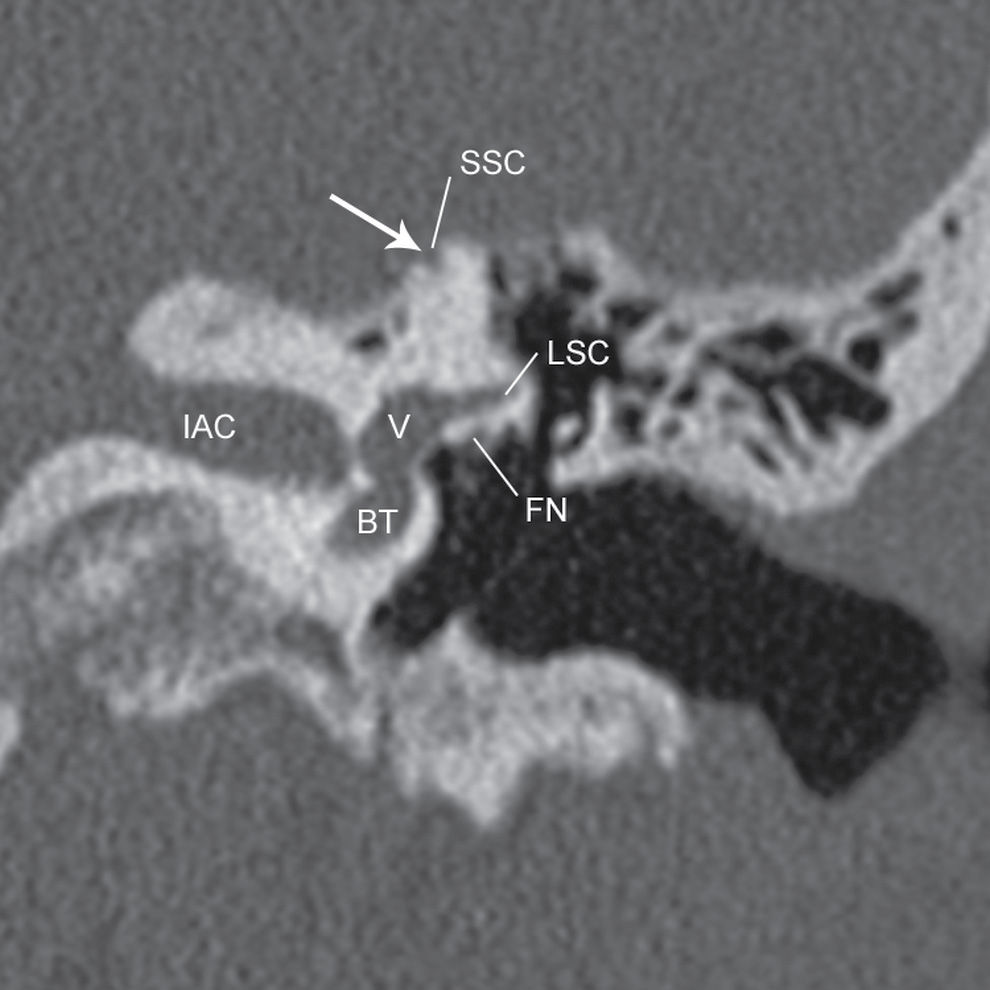
FIG. 20.10 Superior semicircular canal dehiscence. A gap (arrow) is seen in the bony covering of the superior semicircular canal (SSC). The lateral semicircular canal (LSC), facial nerve canal (FN), vestibule (V), and basal turn of the cochlea (BT) are also labeled on this image.
Middle Ear Masses
Cholesteatoma
Cholesteatoma is an expansile erosive lesion lined by keratinizing stratified squamous epithelium (Fig. 20.11). It may result from a congenital inclusion of squamous epithelium in the middle ear cavity (congenital cholesteatoma), or more commonly from abnormal migration of squamous epithelium into the middle ear cavity as a result of chronic infection/inflammation. Erosive enzymes and osteoclast-stimulating agents within the epithelial debris result in bone destruction, the hallmark of cholesteatoma. Classically, acquired cholesteatoma occurs in the setting of an underpneumatized mastoid, involves Prussak space, and erodes adjacent bone, including the ossicles and scutum (6).

FIG. 20.11 Acquired cholesteatoma. Coronal CT shows a middle ear mass (arrow) that grossly erodes the tegmen tympani (TT) and erodes into the lateral semicircular canal (LSC) and facial nerve canal (FN).
When imaging the patient with cholesteatoma, the key features to comment on are the extent of opacification (specifically involvement of the anterior epitympanic recess, round window niche, sinus tympani, or facial recess), integrity of the tegmen tympani, integrity of the facial nerve canal, integrity of the lateral semicircular canal, and regional anatomy relevant to a potential mastoidectomy (e.g., high and dehiscent jugular bulb, or anteriorly positioned sigmoid sinus plate).
Glomus tympanicum
Glomus tympanicum, the most common primary tumor of the middle ear, is a paraganglioma that arises from glomus bodies of Jacobson nerve, a branch of CN IX, along the medial wall of the middle ear cavity. Although glomus tympanicum tumors may occur anywhere along the course of Jacobson nerve, the classic appearance is of a well-defined mass along the cochlear promontory (Fig. 20.12). These lesions show soft tissue density on CT, are mildly T2 hyperintense on MR, and enhance intensely. Although these lesions are very vascular, the typical “salt-and-pepper” appearance of a vascularized lesion is often not seen unless they are very large. The typical clinical history is pulsatile tinnitus, and CHL is also common (9).
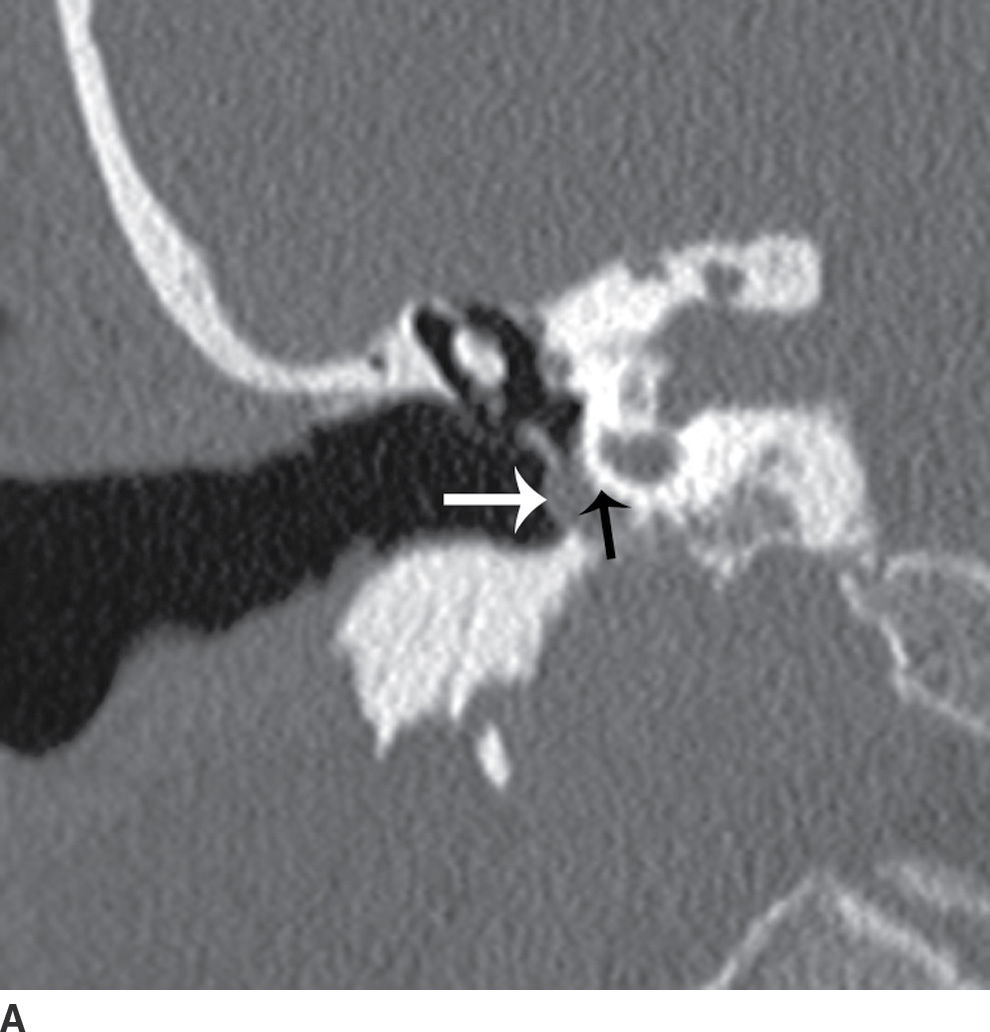
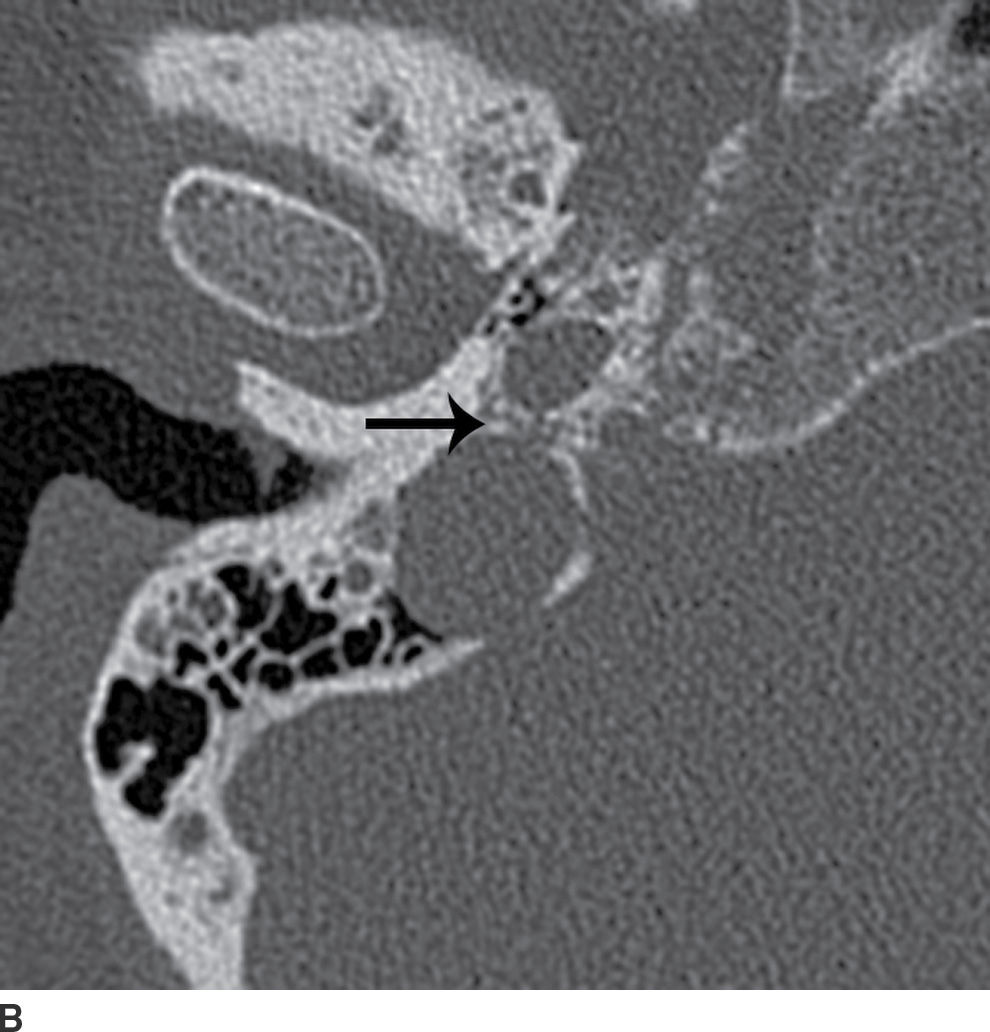
FIG. 20.12 Glomus tympanicum. A: Coronal CT shows a well-defined mass (white arrow) in the anterior hypotympanum. Note the characteristic location along the cochlear promontory (black arrow). B: Axial CT through the skull base shows bone erosion about the caroticojugular spine (arrow), indicating paraganglioma involving the proximal course of Jacobson nerve in the inferior tympanic canaliculus.
When imaging the patient with suspected glomus tympanicum, the job of the radiologist is to first exclude an alternative lesion such as aberrant ICA or high jugular bulb and next to determine whether the lesion is confined to the middle ear cavity or whether the middle ear tumor is a projection of a larger glomus jugulare tumor arising in the jugular fossa (i.e., “glomus jugulotympanicum”). As with any middle ear mass, it is always helpful to comment on regional anatomy that influences the surgical approach.
Jugular bulb dehiscence and diverticulum
The jugular bulb and jugular fossa have variable anatomy. When the jugular bulb is high and has a dehiscent bony covering, it may protrude into the middle ear cavity and produce a bluish mass along the posteroinferior quadrant of the tympanic membrane. This is a normal variant and is only relevant to the extent that it interferes with tympanostomy tube placement or mastoidectomy or simulates other lesions.
Unlike an enlarged or high-riding jugular bulb, a jugular bulb diverticulum is a true venous anomaly. It is defined as an outpouching of the jugular bulb into the petrous bone. Clinically, patients may complain of pulsatile tinnitus, which occurs as a result of turbulent flow passing by the diverticulum. Sigmoid sinus diverticulum results in a similar clinical presentation. CT will demonstrate an expansile, smoothly marginated, enhancing mass.
Aberrant internal carotid artery
An aberrant internal carotid artery (ICA) forms as a result of failure of the cervical ICA to develop. This results in a rerouting of circulation through the inferior tympanic artery and caroticotympanic artery, which course posterolateral to the expected course of the normal cervical ICA, later joining with the distal, normal segment of the intracranial ICA (Fig. 20.13). On CT, the ICA will have an unusual posterolateral location, with deficient bony covering, and will often be smaller than normal. CTA and MRA reveal a focal, posterolateral “knuckle”-like deviation of the ICA. Patients may present with pulsatile tinnitus, or with CHL from the space-occupying effect of the artery in the middle ear (10). Glomus tympanicum and aberrant ICA both present clinically as a pulsatile middle ear mass, and radiologic evaluation is critical for differentiating them, as management is quite different. Aberrant ICA is also associated with persistent stapedial artery (PSA). Absence of foramen spinosum, which normally transmits the middle meningeal artery, is a classic finding in cases of PSA.
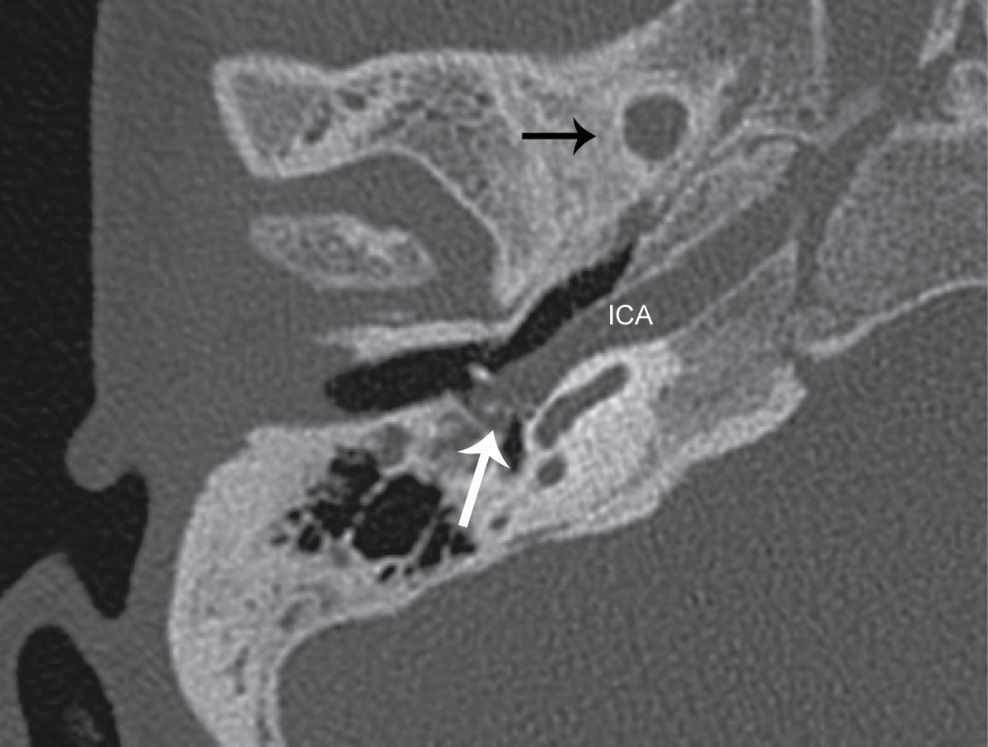
FIG. 20.13 Aberrant internal carotid artery (ICA). Axial CT shows a soft tissue density mass (white arrow) in the middle ear cavity. Note the posterolateral deviation and deficient bony covering of the ICA. No foramen spinosum is seen (black arrow denotes its typical location), suggesting a persistent stapedial artery, which can co-occur with aberrant ICA.
Cerebellopontine Angle Masses
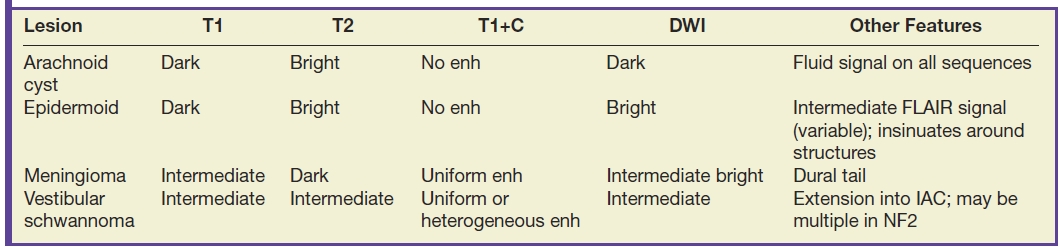
Masses of the cerebellopontine (CP) angle are difficult to detect by CT, but fortunately lend themselves well to evaluation by MR. Every resident should be aware of the four most common lesions in this area and how to readily distinguish them. Table 20.2 summarizes these lesions.
Table 20.2 Cerebellopontine Angle Masses
Vestibular schwannoma
Vestibular schwannoma, previously called “acoustic neuroma,” typically arises from the superior or inferior vestibular nerve near the porus acusticus and may present with tinnitus, high-frequency SNHL, or symptoms related to mass effect. Vestibular schwannomas will grow into the IAC and into the CP angle cistern by varying degrees (Fig. 20.14). On MR, they are heterogeneously hyperintense and enhance intensely with contrast. As with schwannomas elsewhere in the body, they frequently show some degree of cystic degeneration when large. When evaluating the patient with vestibular schwannoma, always look carefully for bilateral lesions, which are diagnostic of type 2 neurofibromatosis. It is also helpful to describe any mass effect on the middle cerebellar peduncle, or extension to the cochlear aperture.
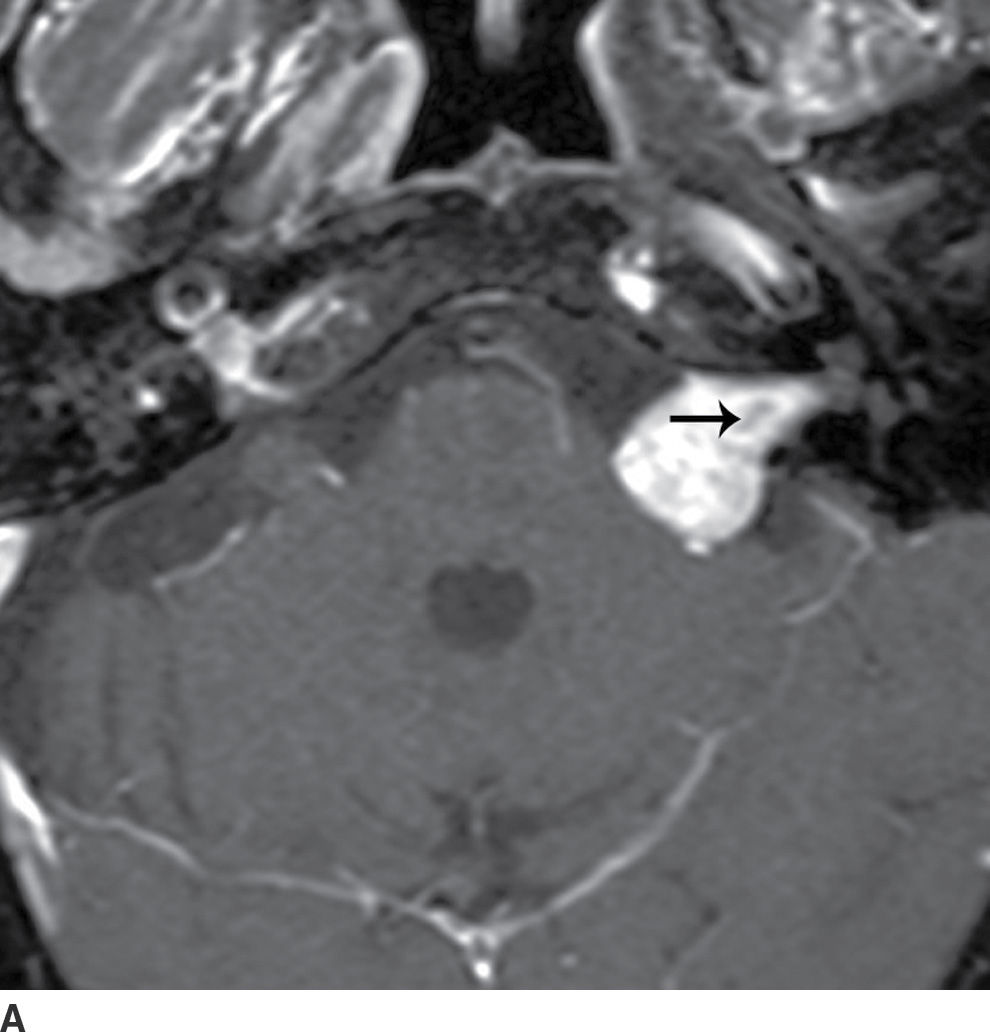
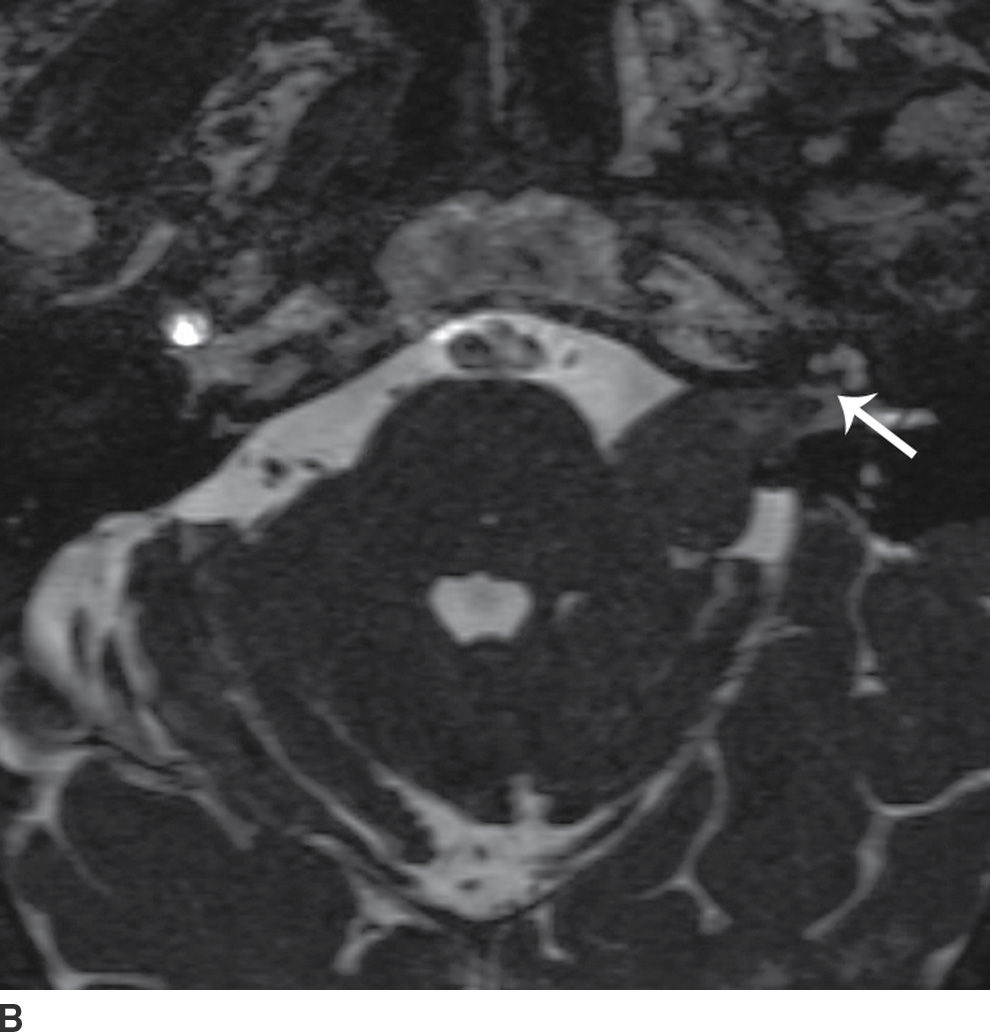
FIG. 20.14 Vestibular schwannoma. A: Axial fat-suppressed contrast-enhanced T1-weighted image shows an avidly enhancing mass that extends into the internal auditory canal and has internal cystic change (arrow). B: Axial cisternographic T2 best depicts the relationship between the most lateral extent of the lesion (arrow) and the cochlear aperture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree