Fig. 1
A large cyst with predominantly hyperechoic contents
Fig. 2
A large cyst with predominantly hyperechoic contents
Management and Prognosis
As these tumours are by definition benign, their prognosis is very good.
Traditional practice recommends removal on the grounds that this prevents torsion and malignant transformation. However, many small MCTs found incidentally on transvaginal ultrasound can be managed conservatively and if slow growing are unlikely to cause clinical symptoms [6, 7, 12]. Factors which increase the likelihood of women managed expectantly then choosing to have surgery include multiparity, young age, larger cysts, bilateral cysts and past history of ovarian cyst [12]. Larger symptomatic cysts may need excision by the open or laparoscopic route. If predominantly cystic, these cysts can usually be managed laparoscopically, but care needs to be taken to avoid spillage of the contents into the abdominal cavity as this can stimulate a peritonitic reaction [16]. The use of endoscopic retrieval bags can help to minimise this. As small asymptomatic cysts are being found with increasing frequency, these are increasingly being managed conservatively with success [6, 7] (Fig. 3).
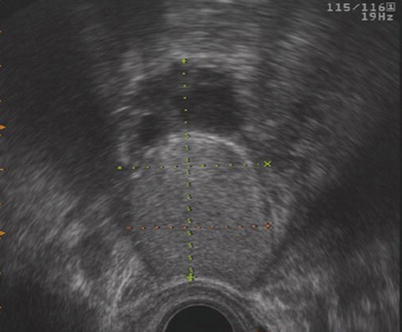
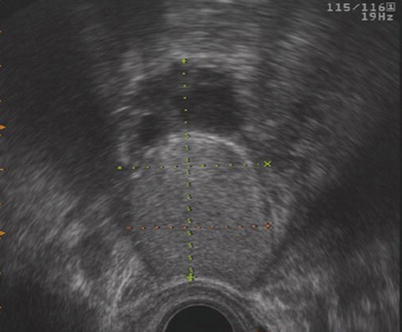
Fig. 3
A medium sized cyst with normal ovarian tissue
Macroscopic Examination
MCT is bilateral in between 10 and 15 % of cases [1]. Multiple teratomas are seen in the ipsilateral ovary in less than 1 % of cases [10]. The tumours are round or ovoid and range in size from 1 to 30 cm, but most are within the 5–10 cm diameter range [25]. They have thick white capsules, which are usually free of adhesions. They are usually unilocular cysts filled with thick greasy sebaceous material and matted hair [25]. These sometimes round up to form sebum and hair balls (Figs. 4 and 5). The sebaceous contents have a fluid consistency above 35 °C which becomes doughy or solid at room temperature [11, 32]. Some cysts however are filled with predominantly mucoid or clear fluid. Most are unilocular, and between 5 and 10 % are multilocular. In 87 % of cases [11], a protuberance can be seen projecting into the cyst cavity called a dermoid protuberance (or Rokitansky tubercle/dermoid mamilla) [32]. The cyst lining is usually smooth like skin and the hair generally grows from this tubercle. Teeth are present in up to one third of cases. Other tissues commonly identified are cartilage, bone, brain and adipose tissue. Older lesions may exhibit marked dystrophic calcification [25]. Hemangiomas are unusual and give rise to highly vascular structures [11]. More organised structures such as intestine; skeletal parts, especially jaw bone; and eyes may be present [25] (Figs. 6 and 7).
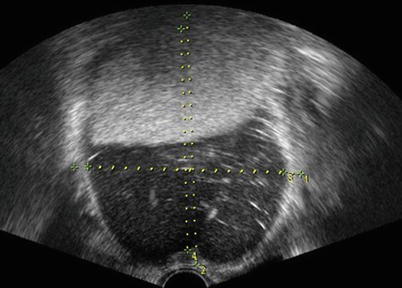
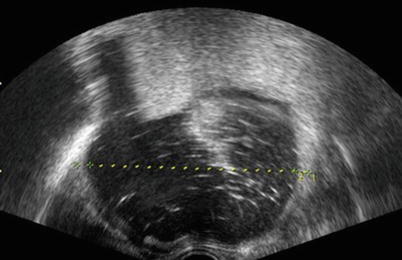

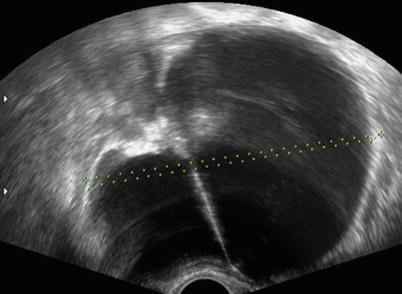
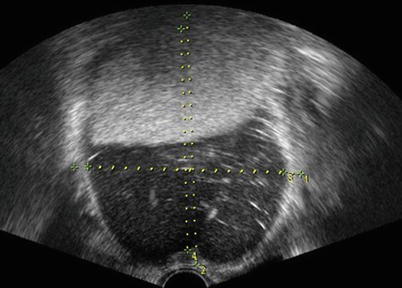
Fig. 4
Sebum, half low level echogenic fluid with “hair” flecks
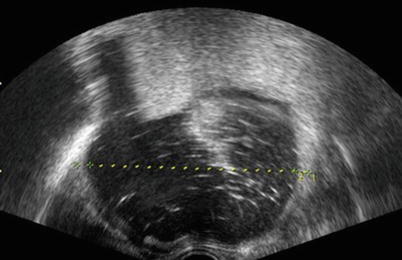
Fig. 5
Half sebum, half low level echogenic fluid with “hair” flecks

Fig. 6
Anechoic fluid with a few hair flecks but no sebum
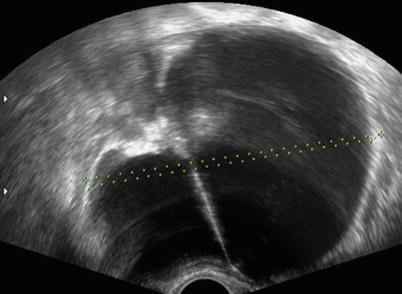
Fig. 7
Anechoic fluid with a single septum and hyperechoic tubercle
Microscopy
Typically, the inner surface of the cyst is lined by epidermis which desquamates into the lumen [11]. Skin adnexal structures such as hair follicles and sebaceous and sweat glands are often present on the dermal papilla [25] and a large amount of mature tissues are usually found at and around this area [11]. Other ectodermal derivatives such as cerebrum, cerebellum, choroid plexus and retina may also be found [24]. The most common mesodermal derivatives are smooth or striated muscle, adipose tissue, bone, teeth and cartilage. Less common tissues are thyroid, peripheral nerve, respiratory and gastrointestinal epithelium, teeth and salivary gland [25].
Ultrasound Features of Mature Cystic Teratomas
Transvaginal ultrasonography has an established role in the evaluation of adnexal masses and provides an accurate assessment of ovarian morphology. It is also well known that dermoid cysts have distinct sonographic grayscale morphological features, which can be used to accurately diagnose dermoid cysts (‘pattern recognition method’) [14, 33–35] (Figs. 8 and 9).
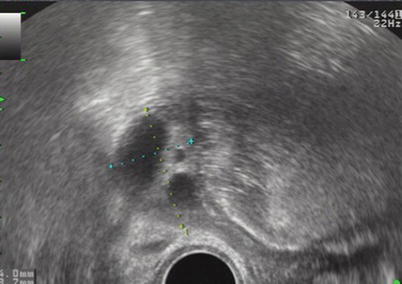

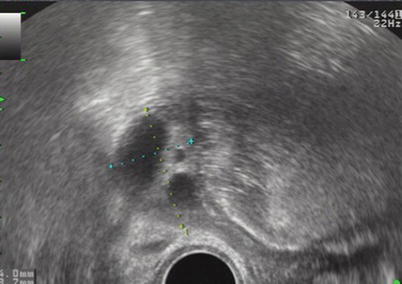
Fig. 8
Healthy ovarian tissue with follicles (The ovarian cresent sign)

Fig. 9
Healthy ovarian tissue with follicles (The ovarian cresent sign)
Previous studies examining the ultrasound morphology of MCT have tried to analyse the appearance of the whole tumour. Laing et al. [18] in 1981 analysed 51 MCTs and found that ‘33 % of the cases demonstrated “typical” findings, i.e. “an echogenic focus with acoustic shadowing in a predominantly cystic mass”, 23.5 % were predominantly solid, 20 % were almost entirely cystic, and 23.5 % were not visible’ on ultrasound scan (Fig. 10). Bronshtein used an in vitro simulation with hair and oil in a glove and showed that this replicated the ‘white ball’ of dermoid very well. They also showed that hair in water can produce the same ‘dot and dash’ echo pattern seen in some dermoid cysts. Cohen [8] in 1993 and Caspi [5] in 1996 attempted to categorise the morphology of MCT into different groups based on the presence of acoustic shadowing and the amount of echogenic material within the cyst cavity. It is our opinion that this approach is rather complicated and that once individual features of hair or sebum are recognised, these alone are sufficient to make a diagnosis in the vast majority of MCT.
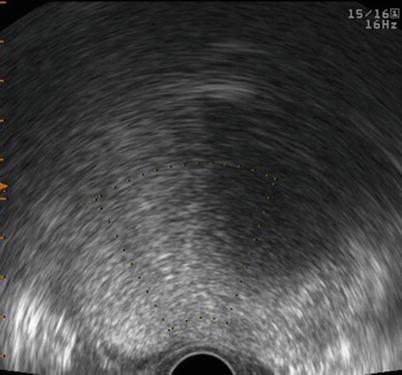
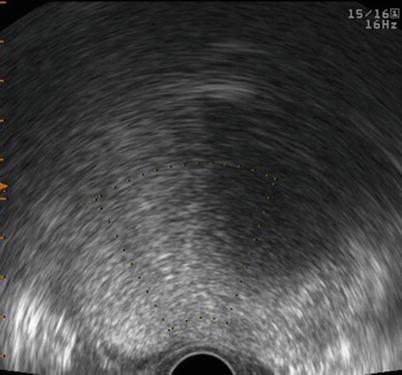
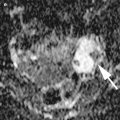
Fig. 10
Acoustic shadowing
Immature Teratomas
Immature teratomas, in common with the mature teratomas, contain tissues from the three germinal layers, but in contrast to mature teratomas, they contain immature or embryonal structures [31]. These tumours arise from postmitotic germ cells and contain immature (embryonal) structures as well as mature elements in most cases [13]. The additional presence of other malignant germ cell tumour elements places the tumour in the teratomas group, and these are excluded from this study. Pure immature teratomas are rare tumours which comprise <1 % of ovarian teratomas overall [15, 22, 31, 32, 37]. They represent 20 % of malignant germ cell tumours and approximately 1 % of malignant ovarian tumours [3] and account for up to 25 % of malignant ovarian tumours presenting in girls <17 years of age [4].
Clinical Presentation
These tumours present between <1 and 58 years of age with median of 18–19.5 and a mean of 20.6 years [4, 19, 22, 23]. Most patients present with an abdominal mass (80 %), approximately half with pain and a quarter with bleeding irregularity (except in premenarchal patients) [22]. These tumours rarely present in pregnancy or as incidental findings in asymptomatic women. Raised α-fetoprotein levels may be present in 60 % of patients and raised β-HCG outside pregnancy may signal a mixed malignant germ cell tumour [15].
Prognosis and Management
The prognosis depends on grade of tumour in stage 1 and grade of metastasis in stage 2–4. Low-grade stage 1 tumours may be cured with excision alone and have a survival rate of 95 % if chemotherapy is used for recurrences [23]. Higher-grade and higher-stage tumours benefit from chemotherapy, and their survival rates have been reported as less than 82 %. Modern improved chemotherapy may offer improved survival rates. Management is with conservative fertility-sparing surgery for low-grade stage 1–2 tumours. In higher-grade stage 1 and 2 tumours and any grade stage 3 tumours, chemotherapy is recommended [25].
Macroscopic Features
These tumours are almost always unilateral unless they present with widespread disease [23], but in 5–10 % of patients, a contralateral mature cystic teratoma is present [23, 38]. Local spread is local peritoneal spread, spread to the omentum, etc., or via lymphatic spread to retroperitoneal, para-aortic, mesenteric and mediastinal nodes [23, 38]. ITs are large tumours presenting with a mean diameter of 16–20 cm and a range of 5–42 cm [23, 38] and a mean weight of 1,300 g (range 22–7, 150 g).
The tumours are predominantly solid although there are usually multiple small cysts of less than 1 cm in diameter present; however, occasional larger cysts may be present [25]. Some contain sebaceous material or hair, but most are degenerative in type and filled with clear mucoid or blood-stained fluid [25]. Solid areas with haemorrhage or necrosis are common and are important as these are more likely to contain the less well-differentiated tissues [4, 23, 25] (Fig. 11).


Fig. 11
Fluid level
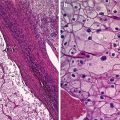
Microscopic Features
All three germinal layers are usually present, and the range of tissues includes all those that may be observed in mature cystic teratomas. The ectodermal and mesodermal components predominate, and it is in these areas that the immaturity is most clearly evident. The various tissues are admixed in a haphazard way, which contrasts with benign dermoid cysts, where the tissues are more organised. Neural tissue may be present and may mimic intracranial malignant tumours. Squamous epithelium may also be present and may show evidence of malignancy. Cartilage and bone may be present. Mesodermal elements show loose fibrous connective tissue which may resemble undifferentiated myxoid embryonic mesenchyme. Smooth—but not striated—muscle is quite common (Figs. 12 and 13).

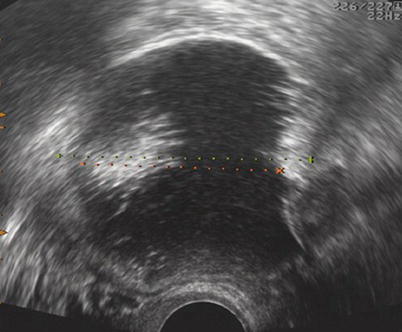

Fig. 12
White ball
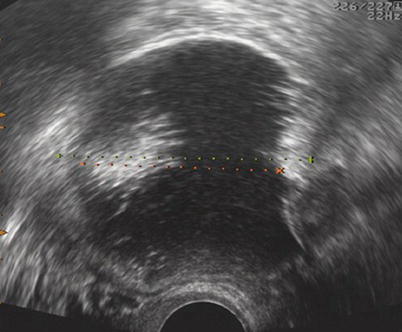
Fig. 13
White ball
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree