George M. Bridgeforth, Jessica Peelman, and Charles Carroll IV
A 15-year-old girl complains of pain in the second digit of her right hand after jamming her finger while catching a baseball.

CLINICAL POINTS
- Volar plate injuries are hyperextension injuries to the finger that are commonly diagnosed as finger sprains.
- Many volar plate fractures are misdiagnosed as finger sprains.
- A history of mechanism and direction of injury aids in the diagnosis.
Clinical Presentation
Volar plate fractures usually involve the proximal interphalangeal (PIP) joint, the most commonly injured area of the hand. The volar plate, a dense band, forms a portion of the capsule (Fig. 44.1). An intact volar plate helps stabilize the joint and prevent hyperextension. The thick ulnar and radial collateral ligaments of the PIP joint combine with the volar plate to supply lateral stability. The PIP joint is especially vulnerable to either ligamentous injury or intra-articular fracture (with or without subluxation or dislocation). Often, there is a small fragment of bone avulsed from the volar aspect of the base of the proximal phalanx.
In volar plate fractures, the mechanism of injury is generally hyperextension or “jamming” of the finger. Volar plate injury may occur with dislocation of the PIP joint.
Clinical signs of a possible volar plate fracture include
- a history of hyperextension to the injured finger,
- moderate-to-marked swelling at the PIP joint,
- tenderness at the volar plate (undersurface of the PIP joint), and
- pain-limited range of motion.
Examination reveals clues to possible abnormalities. Thorough inspection and palpation of the area and localization of the tenderness is important. It is also necessary to check for marked tenderness at the volar (plate) surface of the PIP joint. Maximal tenderness occurs at the volar aspect of the affected joint. In addition, the clinician should test for full flexion and extension by asking the patient to open and close his or her fist. Lateral stressing of the joint evaluates collateral ligament stability.
The differential diagnosis consists of other finger injuries, including finger fractures and contusions. A tenosynovitis (trigger finger) is characterized by diffuse swelling along the fibrous tunic surrounding the finger. Moreover, trigger fingers commonly have decreased range of motion associated with snapping or locking of the finger. The snapping or locking is usually caused by a small fibrous nodule in the flexor tendon. Dislocations of the PIP joint are characterized by marked pain, swelling, and tenderness. Patients not only have impaired range of motion but also a pronounced step-off deformity from the dislocated PIP joint.
Patients with a damaged flexor digitorum superficialis tendon are not able to flex the injured finger at the PIP joint. Patients with a damaged flexor digitorum profundus tendon lack finger flexion at the DIP joint. Damage to the lateral bands at the PIP joint results in varus or valgus instability. Normally, when the proximal phalanx is stabilized with hand, the middle phalanx should not bend internally (varus instability) or externally (valgus instability) when resistance is applied by the examiner. It is essential to check for signs of neurovascular impairment (coldness, cyanosis, impaired pulses or diminished capillary refill of the nail bed, decreased or absent sensation).
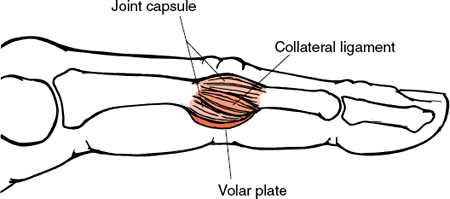
FIGURE 44.1 The supporting structures of the IP joints of the fingers. The supporting structures of the IP joints of the fingers include the capsule, collateral ligaments, and the volar plate. (From Oatis CA. Kinesiology—The Mechanics and Pathomechanics of Human Movement. Baltimore, MD: Lippincott Williams & Wilkins; 2004.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








